Report – Social and economic impacts of COVID-19 on transgender and non-binary people in Canada
A survey led by researchers at Western University explores the experiences of trans and non-binary Canadians during the COVID-19 pandemic. Initial research from the Trans PULSE Canada survey highlighted that many trans and non-binary Canadians will avoid seeking necessary health care because of a fear of discrimination. The survey findings also show that trans and non-binary Canadians had disruptions in primary health care, mental health care and gender-affirming care during the pandemic, and a high frequency of interruptions to hormone regimens. They also found that twice as many trans and non-binary people reported that they stopped accessing mental health support than those who started accessing support. The team also looked at the social and economic impacts of the pandemic and found that a majority of trans and non-binary people in Canada are experiencing negative financial and social impacts of COVID-19. Almost 60 per cent of respondents said they their access to trans and non-binary social spaces has decreased.
Resources
Handouts, slides, and time-stamps
Read the presentation slides for this webinar.
Click ‘Get it’ above for video link for this webinar.
Handout: Implementing a practice of self-care
Impacts of the Covid-19 Pandemic on Women: Report of the Standing Committee on the Status of Women
The effects of the COVID-19 pandemic have been profound and far-reaching. Beyond endangering the health of Canadians, the pandemic has worsened inequalities among groups of people. Women, girls and gender-diverse people have faced unique challenges during the pandemic. The Committee recommends that the Government of Canada take various actions to assist women, girls and gender-diverse people during and after the COVID-19 pandemic. Many recommendations relate to improving women’s health and labour force participation. Some recommendations focus specifically on women’s paid and unpaid care work. The Committee also recommends interventions to help reduce trafficking and violence against women.
The COVID-19 pandemic and Indigenous people with a disability or long-term condition
This paper uses crowdsourced data to provide an overview of the impacts of the COVID-19 pandemic on the health, service access, and ability to meet basic needs of Indigenous participants with disabilities or long-term conditions. Changes in overall health and mental health are examined by disability type, age group and sex. The most commonly reported service disruptions since the start of the pandemic are also presented. The crowdsourcing data reflected health and other disparities between Indigenous and non-Indigenous participants with a disability or long-term condition. Indigenous participants were more likely to report worsened overall health and mental health, service disruption, and a greater impact on their ability to meet essential needs.
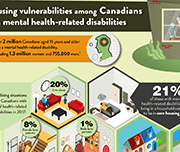
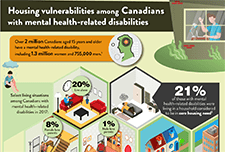
One in five Canadians with mental health-related disabilities lives in core housing need
Canadians with mental health-related disabilities were more than twice as likely as those without disabilities to live in households considered to be in core housing need in 2017. Canadians with mental health-related disabilities were also more likely than those without disabilities to live alone, to rent their homes and to live in subsidized housing, according to the 2017 Canadian Survey on Disability (CSD). The Public Health Agency of Canada (PHAC) has identified those living with pre-existing mental health-related disabilities as a particularly vulnerable population because of the impacts of isolation and disruptions to mental health-related services during the COVID-19 pandemic. A recent crowdsourcing survey by Statistics Canada found that almost three-quarters (73%) of participants with mental health-related disabilities stated that their mental health had worsened since the beginning of the pandemic. In addition, PHAC has indicated that those living with inadequate or unsuitable housing are also more vulnerable during the pandemic and are at higher risk of contracting COVID-19. This infographic presents pre-existing living situations and housing conditions among Canadians with mental health-related disabilities that may put them at greater risk of contracting COVID-19, as well as the emotional and psychosocial impacts of living through a pandemic.
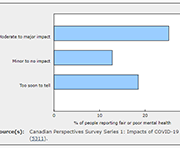
Food insecurity and mental health during the COVID-19 pandemic
Canadians living in households that experienced food insecurity (insecure or inadequate access to food because of financial constraints) during the early months of the COVID-19 pandemic were significantly more likely to perceive their mental health as fair or poor and to report moderate or severe anxiety symptoms than Canadians in food-secure households. Approximately one in seven Canadians (14.6%) were estimated to live in a food-insecure household in May 2020. This study, released in Health Reports, is the first to examine the association between household food insecurity and self-perceived mental health and anxiety among Canadians during the COVID-19 pandemic. The study also estimated that 9.3% of Canadians living in food-insecure households reported having recently accessed free food or meals from a community organization.
The changes in health and well-being of Canadians with long-term conditions or disabilities since the start of the COVID-19 pandemic
This article examines how the self-reported health and mental health of people with long-term health conditions or disabilities has changed since the start of the COVID-19 pandemic explored by age, sex and type of reported difficulty. Additionally, the rates of health service disruptions are explored by type of service and region.
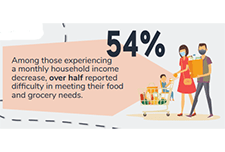
How are Canadians with long-term conditions and disabilities impacted by the COVID-19 pandemic?
This infographic focuses on self-reported health, unmet needs for services and therapies, and difficulties meeting certain financial obligations and essential needs since the start of the COVID-19 pandemic among participants aged 15 and older living with long-term conditions and disabilities. Results are based on the recent Statistics Canada crowdsourcing data collection completed by over 13,000 Canadians with long-term conditions or disabilities between June 23 and July 6, 2020.
The mental health of population groups designated as visible minorities in Canada during the COVID-19 pandemic
This article examines the mental health outcomes (i.e., self-rated mental health, change in mental health since physical distancing began, and severity of symptoms consistent with generalized anxiety disorder in the two weeks prior to completing the survey) of participants in a recent crowdsource questionnaire who belong to population groups designated as visible minorities in Canada.
Canada’s Forgotten Poor? Putting Singles Living in Deep Poverty on the Policy Radar
This report presents the findings of extensive research about employable singles on social assistance undertaken by Toronto Employment and Social Services, in partnership with the Ontario Centre for Workforce Innovation. Drawing on data from 69,000 singles who were receiving social assistance in Toronto in 2016, and 51 interviews with randomly selected participants, the report highlights these individuals’ characteristics, their complex needs, and the barriers they face in moving off social assistance and into employment. Complementing the quantitative analysis, the interviews provide important insights into the daily realities of participants’ lives and their journeys on and off assistance.
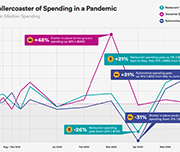
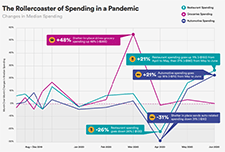
The Economic Toll of COVID-19 on SaverLife Members
SaverLife is an organization that seeks to advance savings programs, analytic insights, and policy initiatives through a network of employers, financial institutions, nonprofits and advocacy groups in the United States. This report provides insight into the financial challenges presented by their savings program members during the COVID-19 pandemic from March to August of 2020.
Hunger Lives Here: Risks and Challenges Faced by Food Bank Clients During COVID-19
This report provides quantitative and qualitative data about the experience of hunger and poverty in Toronto during COVID-19. Based on phone surveys with over 220 food bank clients in May and June 2020 and an analysis of food bank client intake data, the report demonstrates that COVID-19 has led to increased reliance on food banks. The rate of new clients accessing food banks has tripled since the pandemic began. Among new clients, 76% report that they began accessing food banks as a result of COVID-19 and the associated economic downturn.
From Emergency to Opportunity: Building a Resilient Alberta Nonprofit Sector After COVID-19
This report presents an analysis of the impact of COVID-19 on the nonprofit sector drawn from data collected in CCVO's Alberta Nonprofit Survey, data from surveys by the Alberta The analysis in this report shows that the effects on the nonprofit sector have been magnified through increased service demand, decreased revenue, and diminished organizational capacity coupled by delays in support and inadequate recognition for the leadership role that the sector is being called upon to play.
Nonprofit Network, Imagine Canada, and partner organizations across the country.
Canadian Health Survey on Children and Youth, 2019
The current pandemic has reinforced the need for additional information on the health of Canadian children and youth, particularly for those younger than age 12. Results from the new Canadian Health Survey on Children and Youth (CHSCY) indicate that 4% of children and youth aged 1 to 17, as reported by their parents, had fair or poor mental health in 2019, one year prior to the pandemic. The survey also found that poor mental health among children and youth was associated with adverse health and social outcomes, such as lower grades and difficulty making friends. Recently released crowdsourced data suggest that the perceived mental health of Canadian youth has declined during the pandemic, with over half (57%) of participants aged 15 to 17 reporting that their mental health was somewhat worse or much worse than it was prior to the implementation of physical distancing measures.
Shelters for victims of abuse with ties to Indigenous communities or organizations in Canada, 2017/2018
There were 85 shelters for victims of abuse that had ties to First Nations, Métis or Inuit communities or organizations operating across Canada in 2017/2018. These Indigenous shelters, which are primarily mandated to serve victims of abuse, play an important role for victims leaving abusive situations by providing a safe environment and basic living needs, as well as different kinds of support and outreach services. Over a one-year period, there were more than 10,500 admissions to Indigenous shelters; the vast majority of these admissions were women (63.7%) and their accompanying children (36.1%). This article uses data from the Survey of Residential Facilities for Victims of Abuse (SRFVA). Valuable insight into shelter use in Canada and the challenges that shelters and victims of abuse were facing in 2017/2018 is presented.
Infographic: The impact of the COVID-19 pandemic on Canadian families and children
This infographic describes parents' experiences during the COVID-19 pandemic including balancing work and schooling, their children's activities and parents' concerns.
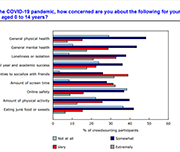
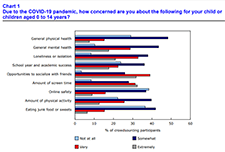
Impacts of COVID-19 on Canadian families and children
The COVID-19 pandemic has dramatically altered the way of life for Canadian families, parents and children. Because of physical distancing and employment impacts, parents have altered their usual routines and supports, and many children and families have been isolated in their homes for months. Children, in particular, may not have left their homes or seen any friends or family members other than their parents for an extended period, since children do not typically have to leave their homes for essential services. However, the impact of the pandemic on families has yet to be described. The purpose of this report is to provide a snapshot of the experiences of Canadian parents and families during this unprecedented time.
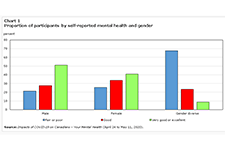
Gender differences in mental health during the COVID-19 pandemic
Previous research has demonstrated that the COVID-19 pandemic is negatively affecting the mental health of Canadians. Today, a new study highlights gender differences in the pandemic's impacts on the mental health of participants in a recent crowdsourcing survey, conducted by Statistics Canada from April 24 to May 11, 2020. Around 46,000 Canadian residents participated in this survey. Female participants were more likely than their male counterparts to report "fair" or "poor" self-rated mental health, "somewhat worse" or "much worse" mental health since physical distancing began, and symptoms consistent with moderate or severe generalized anxiety disorder in the two weeks before completing the questionnaire. Female participants were also more likely than male participants to report that their lives were "quite a bit stressful" or "extremely stressful." Gender-diverse participants—that is, participants who did not report their current gender as exclusively female or male—reported poorer mental health outcomes than both female and male participants across all measures.
Taxpayer Rights in the Digital Age
This paper explores the intersection of digital innovation, digital services, access, and taxpayer rights in the Canadian context, in light of the experiences of vulnerable populations in Canada, from the perspective of the Taxpayers’ Ombudsman. Many aspects of the CRA’s digitalization can further marginalize vulnerable populations but there are also opportunities for digital services to help vulnerable persons in accessing the CRA’s services.
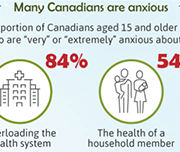
Understanding the perceived mental health of Canadians during the COVID-19 pandemic
While the physical health implications of the COVID‑19 pandemic are regularly publicly available, the mental health toll on Canadians is unknown. This article examines the self-perceived mental health of Canadians during the COVID‑19 pandemic and explores associations with various concerns after accounting for socioeconomic and health factors. Just over half of Canadians aged 15 and older (54%) reported excellent or very good mental health during the COVID‑19 pandemic. Several concerns were also associated with mental health. Notably, after considering the effects of socioeconomic and health characteristics, women, youth, individuals with a physical health condition and those who were very or extremely concerned with family stress from confinement were less likely to report excellent or very good mental health.
COVID-19 and support for seniors: Do seniors have people they can depend on during difficult times?
In an effort to avoid the spread of COVID-19, Canadians are engaging in physical distancing to minimize their social contact with others. However, social support systems continue to play an important role during this time. In particular, seniors living in private households may depend on family, friends or neighbours to deliver groceries, medication and other essential items to their homes. This study examines the level of social support reported by seniors living in private households.
Infographic: How are Canadians coping with the COVID-19 situation?
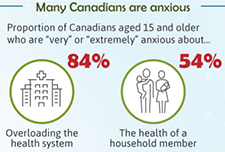
An infographic on the findings from a web panel online survey conducted by Statistics Canada between March 29 and April 3 on how Canadians are responding to the COVID-19 situation. A summary of how many Canadians are feeling anxious, what they are doing during the crisis, and the main precautions that they are taking are presented.
Canadian Perspectives Survey Series 1: Impacts of COVID-19 on job security and personal finances, 2020
Findings from a web panel survey developed by Statistics Canada on how Canadians are coping with COVID-19. More than 4,600 people in the 10 provinces responded to this survey from March 29 to April 3. In addition to content on the concerns of Canadians and the precautions they took to reduce the risk of exposure to COVID-19, the survey includes questions on work location, perceptions of job security, and the impact of COVID-19 on financial security.
Social Prescribing in Ontario
Research has shown that even short-term isolation can have long-term impacts to mental health. Social and community supports are essential for vulnerable persons, especially during times of severe impacts to routine and imposed social distancing. This report discusses the findings of the Rx: Community - Social Prescribing in Ontario pilot, using social prescribing as a tool to better connect social and clinical care and broaden the definition of health and well-being.
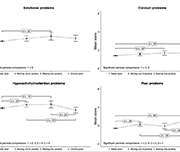
Economic volatility in childhood and subsequent adolescent mental health problems: a longitudinal population based study of adolescents
This research paper investigates the association between the patterns of duration, timing and sequencing of exposure to low family income during childhood, and symptoms of mental health problems in adolescence.
Infographic: New Data on Disability in Canada, 2017
This infographic released from Statistics Canada compiles some of the data collected from the 2017 Canadian Survey on Disability. 22% of Canadians had at least one disability, representing 6.2 million people.
Debt and mental health: A statistical update
Financial problems can be a significant source of distress, putting pressure on people's mental health, particularly if they are treated insensitively by creditors. Some people in financial difficulty cut back on essentials, such as heating and eating, or social activities that support their well being, to try and balance their budget. In many cases this has a negative impact on people's mental health. This policy note from draws on nationally representative data to update key statistics on the relationship between debt and mental health problems, and sets out implications for policymakers, service providers and essential services firms.
In sickness and in health: The association between health and household income
This study uses data from the Longitudinal and International Study of Adults (LISA) to analyze the association between health and household income. Using data on both self-reported general health and self-report mental health, as well as self-reported labour-market outcomes and linked tax records, the association between spouse-pair labour-market income and health is further decomposed into an employment effect reflecting the association between health and the probability of employment, an hours worked effect reflecting the association between health and the number of hours worked, and a wage effect reflecting
the association between health and hourly wages.
Child Welfare and Youth Homelessness in Canada: A Proposal for Action